Training EMS on Our Complex Population
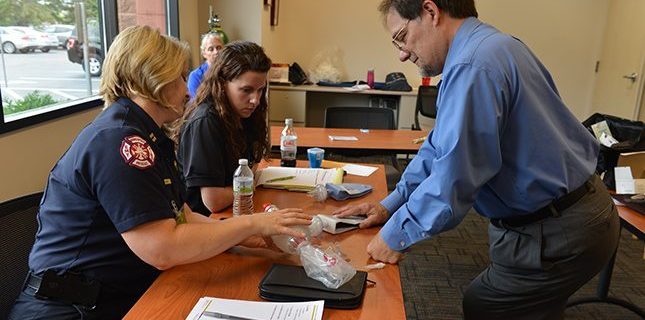
Last month, PHS invited two Hennepin County Emergency Medical Services personnel to come to the office for an afternoon of training on responding to calls for children with tracheostomies and/or central lines. By educating emergency personnel on the needs and special considerations of these children with medical complexities, they will be able to respond more effectively and can enter the home with a better understanding of what to consider when called for an emergency.
Erin Glover, Education Specialist for Emergency Medical Services, and EMS Training Officer Amber Lage learned about infusion basics from our Infusion Nurse Jill Wall, and trach tube essentials from Bruce Estrem, Manager of Clinical Education at PHS. During the session, they also had the opportunity to work hands on with the equipment while relating all of the information directly to situations they may encounter during emergency response.
Training First Responders
Equipped with the information learned during their session at PHS, Erin and Amber will bring the training to First Responders across Hennepin County so anyone responding to a call will be better prepared to react to pediatric medical complexities in the home.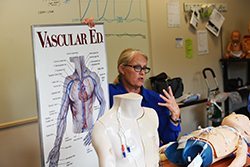
“A lot of times, we’ll get that the patient is short of breath, but that’s it,” mentioned Amber. “Then you walk in and it’s a short of breath trached patient who has a mucus plug. It’s good to know that information in advance, so I know to bring in my suction or start thinking of solutions. I don’t see this scenario often, so it would be good to know what the situation of the child is.”
Training began this month, and will continue to reach personnel across the county.
Information is key
In order to react as quickly as possible once they arrive at the home, it’s helpful for First Responders to know certain pieces of information about the child’s health and general condition. Erin shared some details with us that would be helpful for parents to communicate to responders:
- Who is the primary caregiver when emergency services are called? (sometimes staffing changes are made in the midst of emergencies, day vs night staff)
- What is the patient’s baseline, especially respiratory and mental status? This is usually different from a non-complex child, so knowing what is ‘typical’ is helpful for assessment.

- What specifically is needed from EMS, emergency care vs transportation vs lifting assistance or back up in a power outage?
- PHS encourages families to contact their local fire department before they need them for an emergency to let them know they have a medical complex child in their home in case tornadoes, different outages, etc. occur.
- Have an emergency plan in place specifically for First Responders – often, they are handed a huge binder of all of the child’s medical history and chartings, but they typically need a quick reference of demographic information, diagnosis, allergies, meds, vent/feeding tubes, etc.
- Where is the emergency tool kit kept?
An alert for families
Currently, Hennepin County is in the process of organizing a system in which alerts are set on homes with children that have special healthcare needs (Hennepin County must be notified by parent/guardian for the alert to be added). With this in place, responders will be notified of an alert in the system that will let them know the home they’ve been called to has a child with medical complexities, letting them know what to expect ahead of time.
Once there is an alert system in place, PHS will be sure to update families to let them know how they can submit a note for their address.
“The more information we can have pre-arrival, the better,” added Erin.
Responding to a need
After meeting team memberships from Emergency Medical Services, it became clear that this was a need that could be filled by training the trainers to bring the information back to emergency personnel across the county.
 “Our “all about peds” session started recently with Richfield Fire Department, and the feedback was very good with regards to the station dedicated to children with medical complexities,” said Erin. “Most responders stated these were calls that always sparked the most fear for them, which validates our commitment to educating personnel in the Minneapolis area on this topic.”
“Our “all about peds” session started recently with Richfield Fire Department, and the feedback was very good with regards to the station dedicated to children with medical complexities,” said Erin. “Most responders stated these were calls that always sparked the most fear for them, which validates our commitment to educating personnel in the Minneapolis area on this topic.”
By providing knowledge to anyone who may respond to an emergency call for a child with medical complexities, we know a safe and comprehensive care plan will continue – a mission we are dedicated to each day.
Originally published: October 20, 2015